When people talk to their closest friends about troubles in their lives, the natural tendency is to look only at personal experiences, family problems and relationships. Less commonly, in my experience, do people think about physical illness, biochemical processes, genetics or the brain.
When it comes to dopamine, too little of it and you have Parkinson’s disease; too much, and you have schizophrenia.
One inescapable biological reality is the lump of fatty material sitting serenely in its protective casket on our necks. Solid and yet delicate, the brain is supremely vulnerable and the skull affords only modest protection. It is certainly no match for, say, a car speeding towards you.
We take our raw perceptions and intuitions as given, moment by moment, we have no awareness that there is a brain behind all this, doing the thinking. While philosophers have for centuries picked away at the illusion of unity, it is often only with damage to the brain that we start to notice the join, to see the ‘bio’ and the ‘psycho’ pulling apart.
It was well known that patients with Parkinson’s disease showed degeneration of a small cluster of cells in the midbrain, called the substantia nigra because of its dark colour, which has a high concentration of the chemical neuromelanin, a precursor of dopamine. Those cells feed into the basal ganglia, which is crucially involved in movement control and contains high concentrations of dopamine. The basal ganglia are a small collection of neurons (ganglia) on either side, deep in the base (basal area of the brain).
That theory, the original version of the dopamine hypothesis of schizophrenia, still accounts for many of the facts around schizophrenia. For example, most drugs which produce schizophrenia-like effects have been shown to act via an increase in dopamine transmission and, conversely, most drugs with antipsychotic effects do the opposite: they block or deplete the amount of dopamine in the brain.
We can think of neurotransmitters as being like the baton in a relay race. Nerves convey information in the form of electrical impulses. This is like the runner taking off down the track. Once they reach the end of their leg, they need to pass the baton to the hand of the next runner. The gap between the two runners is analogous to the synapse, a tiny cleft between two nerves. Once the new nerve is safely in receipt of the baton, the message is able to continue further.
As in a relay race, this is a point where flow can be enhanced or disrupted. In Parkinson’s disease there just aren’t enough runners carrying the dopamine baton and not enough batons reach the destination. Dopamine-replacement therapy is like putting out extra batons at the changeover point, increasing the chances that some will get picked up. Other dopamine-enhancing therapies prevent the breakdown of dopamine at the receptors – a bit like allowing stray batons to ‘stay live even if dropped, and permitting runners to pick them up.
As in a relay race, this is a point where flow can be enhanced or disrupted. In Parkinson’s disease there just aren’t enough runners carrying the dopamine baton and not enough batons reach the destination. Dopamine-replacement therapy is like putting out extra batons at the changeover point, increasing the chances that some will get picked up. Other dopamine-enhancing therapies prevent the breakdown of dopamine at the receptors – a bit like allowing stray batons to ‘stay live even if dropped, and permitting runners to pick them up.
Dopamine transporter scan. This involves injecting a tiny amount of a radioactive tracer into the patient’s vein, which allows us to see the special transporter proteins that tidy up stray dopamine molecules when we do the scan. In a healthy brain, there is supposed to be a ‘hot spot showing a concentration of dopamine transporter in the basal ganglia.
It should appear as normal for people who have only drug-induced symptoms of Parkinson’s, whereas people with real Parkinson’s disease have a weaker and cooler hot spot. Early in the disease, production of the transporter falls; after all, you don’t need so many transporters if the amount of dopamine has dropped dramatically.
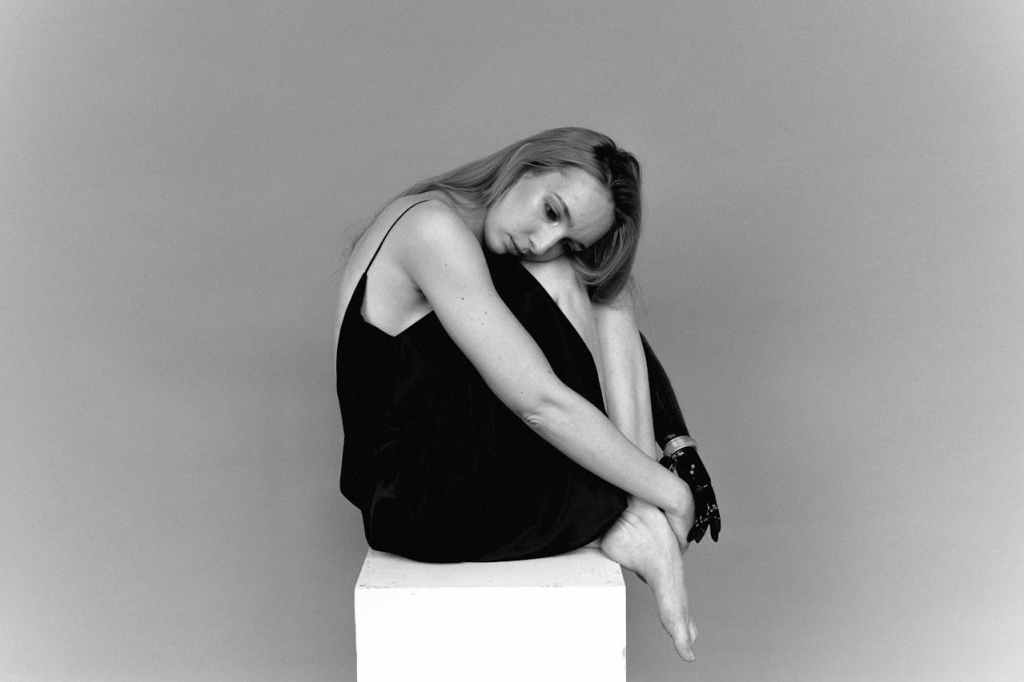
‘Catatonia’ is a broad term that encompasses a group of strange motor behaviors mainly characterized by lack of movement (or speech) or the maintenance of an abnormal posture. Descriptions in old textbooks talk of moving the person’s limbs and them feeling like a tailor’s dummy (‘waxy flexibility’) – staying in whatever position they are left in. Often the person stares ahead eerily, blinking infrequently.
Forms of catatonia describe when a patient who is otherwise mute repeats exactly what is said to them (echolalia’), or the movement equivalent when, despite being otherwise motionless, they seem to mimic the examiner’s actions (‘echopraxia’). Catatonia is not a diagnosis in its own right and may be seen in people with schizophrenia but also severe affective disorder, when their mood is extremely low (as in stupor) or extremely high (as in mania). It can also occur as a reaction to extreme stress or interpersonal conflict.
Source : Into the Abyss: A Neuropsychiatrist’s Notes on Troubled Minds by Anthony David
Goodreads : https://www.goodreads.com/book/show/52386552-into-the-abyss
Read Next Article : https://thinkingbeyondscience.in/2025/04/10/exploring-the-role-of-memory-in-recognition-and-emotion/






Leave a comment