Depression is often misunderstood, leading to stigma and delayed help. Many myths confuse normal sadness with this medical condition, but distinguishing them is crucial for getting the right support. Let’s break down the facts.
Myth 1: Any Prolonged Sadness Means Depression
Fact: Being sad isn’t the same as having depression. Depression is a diagnosed medical illness based on specific symptoms lasting at least two weeks. These can range from mild to severe and include:
- Feeling sad or having a depressed mood
- Loss of interest or pleasure in activities once enjoyed
- Changes in appetite, leading to weight loss or gain unrelated to dieting
- Trouble sleeping or sleeping too much
- Loss of energy or increased fatigue
- Increase in purposeless physical activity (like handwringing or pacing) or slowed movements and speech (observable by others)
- Feeling worthless or guilty
- Difficulty thinking, concentrating, or making decisions
- Thoughts of death or suicide
The UK’s National Health Service (NHS) adds signs like continuous low mood, hopelessness, low self-esteem, tearfulness, guilt, irritability, and lack of motivation. If these persist for weeks or months and disrupt work, social, or family life, seek professional help like psychotherapy to address root issues early.
Myth 2: You Can Will Depression Away by Staying Positive
Fact: Advice like “snap out of it” or “just go for a run” implies depression is a choice. You can’t will it away any more than a cold or fever—just like those, it requires treatment such as medication and/or psychotherapy, plus support. Well-meaning suggestions overlook this reality.
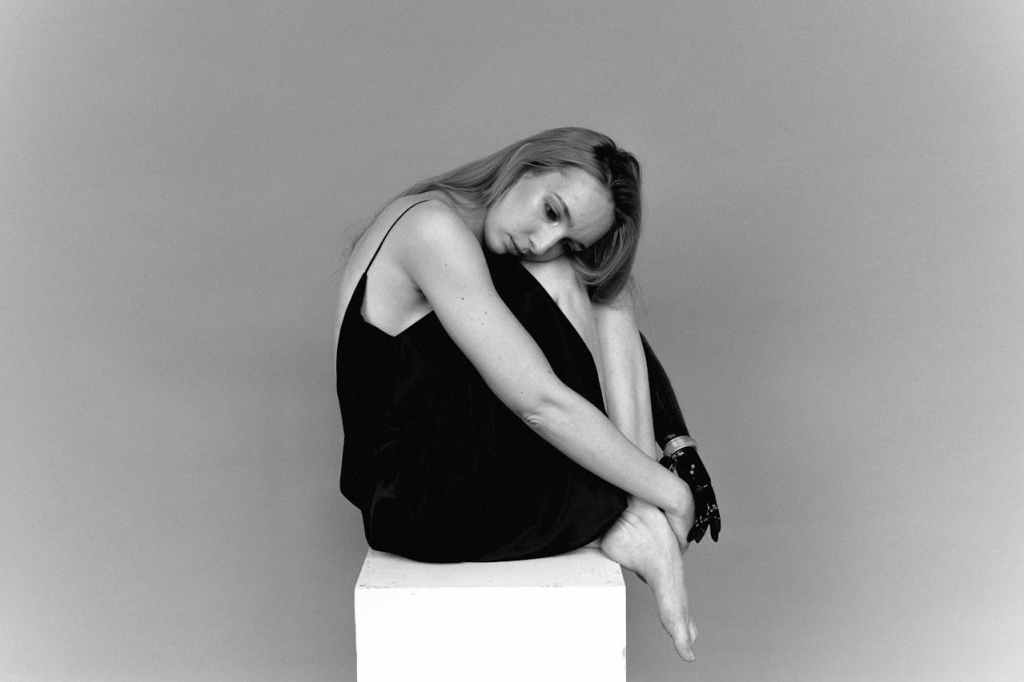
Myth 3: Depressed People Always Look the Part
Fact: Many with depression don’t show outward signs. They go to work, attend social events, and manage daily life while suffering internally. This is common in high-functioning depression, where people stay active but battle underlying sadness triggered by stress. They cope by burying themselves in work, staying busy, exercising, or talking to loved ones, but the struggle remains real and can overwhelm.
Myth 4: Overthinking Causes Depression
Fact: Causes include brain chemistry, genetics, and environmental factors—often a mix. Over-analyzing doesn’t create it. Family history plays a big role: up to 40% link to genetics, and those with depressed relatives are three times more likely. Other triggers include big life events (like divorce, job loss, or childbirth), substance abuse, or illnesses like heart disease, cancer, or diabetes.
Myth 5: Antidepressants Are the Only Fix
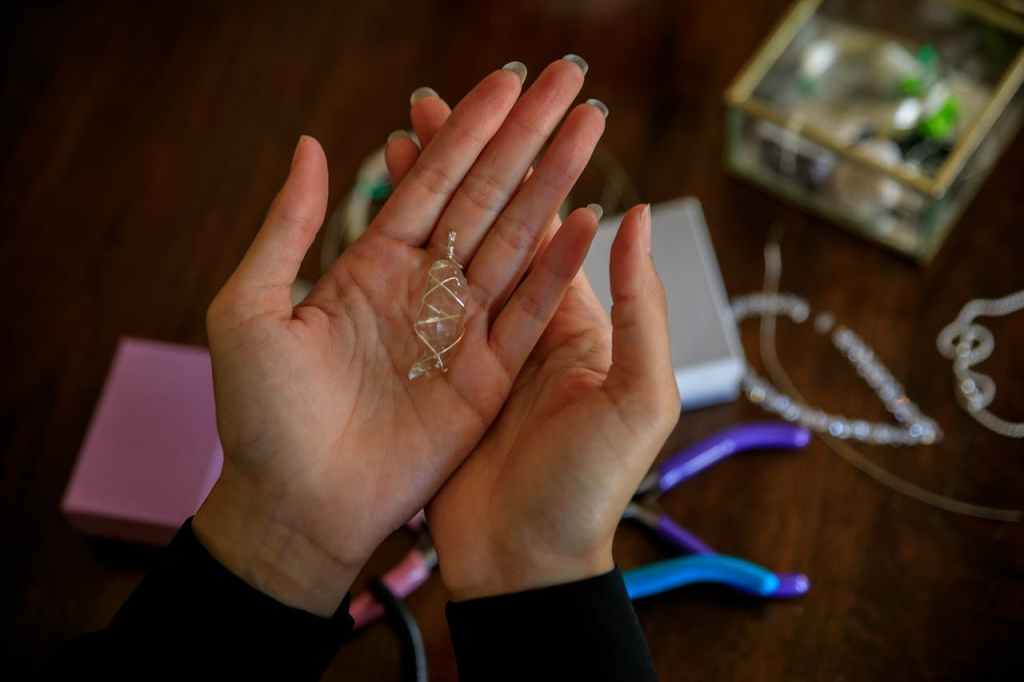
Fact: Treatment is personalized, combining medication (for severe cases affecting daily function) with psychotherapy. An evaluation considers symptoms, history, culture, and environment for a tailored plan. We’re all on a mental health continuum—some in deep despair, others with steady low-grade sadness, like comedian Jessie Klein’s quip about “being a little bit sad all the time.” Building insight helps develop healthier coping.
Supporting Loved Ones with High-Functioning Depression
Families often struggle to spot it. The person needs to communicate openly. Families can help by:
- Allowing space and time to focus on personal needs
- Offering support through outreach, listening, or availability
- Encouraging professional help for both the individual and family to learn better strategies
Understanding these myths empowers us to recognize depression’s many faces and act before it worsens. If symptoms resonate, talk to a professional—early steps make a difference.
Source : Real stories of dealing with Depression: Mindscape series by Amrita Tripathi
Goodreads : https://www.goodreads.com/book/show/46212299-real-stories-of-dealing-with-depression
Read the Previous Article in the Series :





Leave a comment