The human brain is like a dense forest canopy, with conscious thought – the cognitive brain – in the treetops and the emotion of the visceral brain in the branches all converging down towards the trunk – the reptilian brainstem. The memory had risen up from the interacting elements of this concealed space.
We are the sum of our memories. They shape our understanding of the world, connecting us to our past and the people closest to us. Memories can also be our undoing. Most traumatic memories fade, their sharp edges dulled by time. When they remain undimin-ished, however, they can haunt us. They can disrupt our daily lives, making us unable to focus or function.
These intrusive memories germinate after trauma, sprouting and growing pernicious roots. Like some unwanted and malevolent visitor from the past, they arrive uninvited and do not let us forget. The way we deal with these traumatic memories is vital, because we’re unlikely to make it through life without avoiding trauma entirely.
Experiencing trauma is a by-product of the human condition. Most of us have had or will have a traumatic event in our lives. For many of us, it will be multiple traumas. The best estimates suggest that roughly three quarters of people worldwide have experienced at least one traumatic event. We’ve witnessed a death or a grave injury, been assaulted, suffered a life-threatening illness or experienced the unexpected death of a loved one.
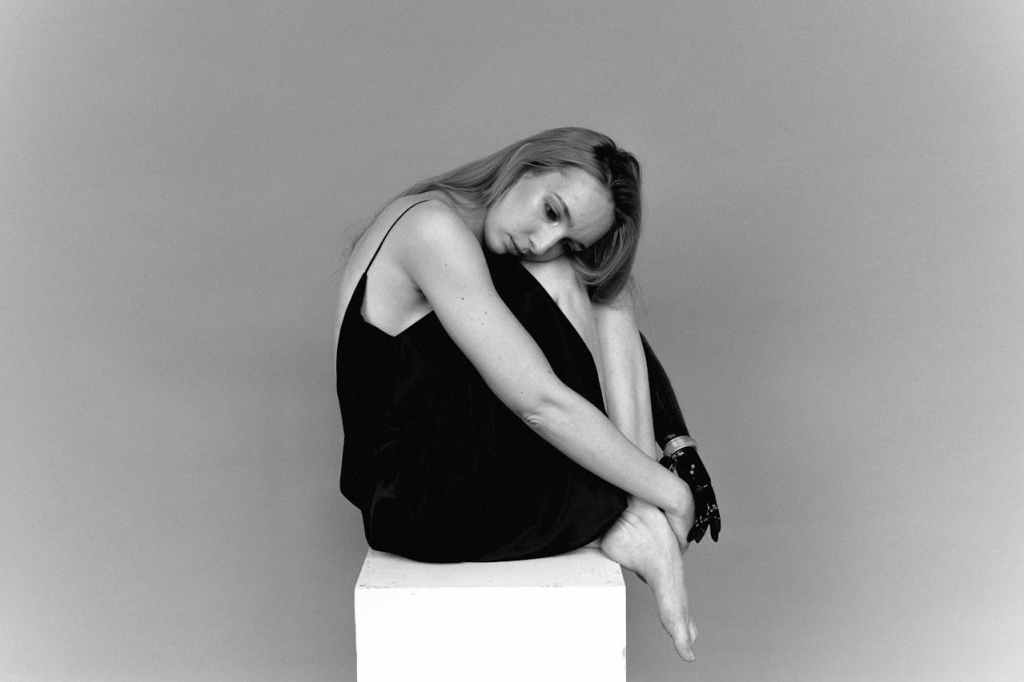
When a trauma victim wakes up, it’s already hap-pened: ribs sliced, bowels rerouted, brain lobes removed, limbs amputated. At first, they are often groggy and not fully aware. The mix of narcotics and the realization that they have survived is almost always met with relief, even by some who attempted suicide. They don’t have the foresight to know the long journey ahead to becoming physically independent and free from the aftershocks of what they ve been through.
Once they are out of the intensive care unit (ICU) or on lower doses of drugs, I begin to see differences in people. And it’s not just about whether they have social support systems or resources. It’s about whether a poisonous emotion takes hold – guilt. If what happened was out of their control, the patients are thankful to be alive and direct their emotions and their grief out-wards, to fate, to someone or something else, but rarely inwards, at themselves. However, if it was an error in their judgement that led to the trauma – for example, they hadn’t been wearing a seat belt – patients struggle with inwardly directed guilt and shame, a sense that ‘I did this to myself.’
If you’re struck by a hammer or fall on your head, the flesh of your brain reacts immediately at a cellular level. Neurons are surrounded by allies called glia, which protect them so the injury doesn’t spread to neigh-bouring healthy neurons, like falling dominoes. Like the neurons themselves, these glia are precious. Their response to an injury, the way they surround and protect the neurons, is called gliosis. It looks like a scar, visible to the naked eye during brain surgery: a dull, yellowish rim around the opalescent white brain. Gli-osis protects the surrounding brain from injury, but only for a while. In time, it may become the origin for aberrant incoherent electricity – seizures. So, at a biological level your immediate response to trauma is protective but, over time, it gets in the way. At a behav-ioural level, the same thing can happen. The trauma can return in overwhelming ways, the aftershocks upending and intruding on the patient’s world, causing depression, profound anxiety, or some uniquely personal and painful combination causing Post Traumatic Stress Disorder (PTSD).
PTSD is not based on a blood test or some other objective measure but on a set of observations; it’s a shorthand for the specific misery some people experience in the aftermath of trauma. The abbreviation has become part of the popular lexicon, watered down, simplified, trivialized to describe our reactions to the hassles and discomforts of everyday life. What the diagnosis sets out to describe, however, is anything but trivial. It is characterized by three sets of persistent symptoms: re-experiencing the trauma through flashbacks and nightmares; avoiding emotional attach-ments; and hyperarousal, which can cause sufferers to startle easily, to feel on edge and anger quickly.
Common perceptions of which gender or type of person is prone to PTSD don’t tell a nuanced story. For example, some soldiers experience PTSD without ever going into combat, and after sexual trauma, men have a higher incidence of PTSD than women.
For most people suffering from trauma, their symptoms don’t conform to a tidy checklist; they defy easy classification. But their suffering is no less real for that. By definition, PTSD requires physical trauma, but emotional trauma can cause the same devastating symptoms as physical trauma and bring the same unbidden vigilance and intrusive memories.
With so much coming at us, our brains are built to forget far more than we remember. They have evolved to understand the world in broad brushstrokes, not to remember each pixel from the past. Forgetting most of the flotsam and jetsam of everyday life – a phone number or where you parked the car yesterday – helps us remember what’s important. It’s called adaptive for-getting. Most memories fade, like an old photograph, losing their emotional punch, along with many of the details, but memories of a trauma can last, and mental images of a trauma can reappear, unwanted – the attacker’s plaid shirt or the red car just before it hits you. Trauma can make us fearful of the people, places and objects that were present when it occurred.
Source : Life on a Knife’s Edge: A Brain Surgeon’s Reflections on Life, Loss and Survival by Rahul Jandial
Goodreads : https://www.goodreads.com/book/show/58248108-life-on-a-knife-s-edge
Read Next Article : https://thinkingbeyondscience.in/2025/05/20/understanding-emotional-memory-the-key-to-post-traumatic-growth/






Leave a comment